HEART RHYTHM SPECIALIST

Atrial Fibrillation: Q&A
You can download a powerpoint presentation covering general aspects about AF here. Atrial fibrillation treatment options.ppt. This is a large file (18 MB) so the download may take a while depending upon the speed of your internet connection.
You can download a PDF file for the content of this page by clicking on Atrial Fibrillation.pdf.
Atrial Fibrillation (AF, or Afib) is the commonest rhythm disturbance affecting humans, and affects more than half a million people in the UK alone. AF starts to become increasingly prevalent after the age of 50 years, and 10% of the over-80s have it. It can occur at an even younger age, especially in the presence of predisposing factors like high blood pressure or heart disease.
Q. What is AF?
In normal hearts, the top two chambers (‘atria’) pump blood in a coordinated fashion into the two bottom chambers (‘ventricles’) which then pump this blood to the rest of the body. This normal relationship is maintained by a well defined electrical impulse (normal sinus rhythm) occurring at the rate of between 60 and 100 beats per minute.
In AF, the normal electrical impulse in the 2 atria is disrupted and is replaced by totally chaotic electrical activity. The Atria now ‘fibrillate’ at a rate of 300-400 times a minute and the ventricles follow in a fast irregular fashion at rates upto 200 beats per minute.
Q. What causes AF?
For years, AF was a poorly understood arrhythmia. Now we know that in most cases, AF is caused by rapidly firing electrical impulses from one or more of the 4 pulmonary veins, the tubes that drain blood from the lungs into the heart.
See CT image of the heart on the right for an illustration.
-
Q.What conditions predispose to AF?
Firstly there are the well known causes like Hypertension, Ischemic heart disease (‘heart attack’), and diseases of heart valves. These do not account for all cases of AF however, and there is a large minority of cases of unknown origin that fall into the category of ‘Lone AF’. We have recently begun to appreciate that even these ‘Lone AF’ patients have predisposing factors like obesity, obstructive sleep apnoea (excessive snoring during sleep) and borderline high (and hence not treated) blood pressure. It is also notable that AF affects athletes and ‘large people’ (who are not necessarily obese) disproportionately. The exact reasons for this are unclear.
Q. How does AF affect heart function?
Firstly, AF results in total loss of atrial contraction. This means that 2 of the 4 heart chambers do not contribute to its working at all resulting in a decrease in heart function by almost a third. This causes symptoms of fatigue and shortness of breath. While patients may not notice this reduced heart function when they are resting, they struggle to cope in periods of increased demand as during exercise. In fact, patients with AF often describe their heart function as ‘an engine that seems to have lost its turbo charger’.
Secondly, when the atria do not contract, blood swirls around in them rather than transiting through them quickly. This increases the chance of blood clots forming which in turn can shoot off and cause stroke. AF increases the risk of stroke 5 fold, and in fact, AF is the commonest cause of stroke worldwide.
Thirdly, the fast and erratic heart rates caused by AF can wear the ventricles out over time and predispose to tachy-cardiomyopathy. In this condition, the heart muscle itself grows weaker and flabbier.
For these reasons, several large population based trials have shown a strong association between AF and increased risk of premature death. They have shown that AF can dock between 5 and 10 years of your life span.
Q. If AF can be so serious, why hasn’t it received due importance?
Historically this has been due to two main reasons. Firstly a lot of the dangerous effects of AF are insidious, and take years to develop. Unlike say a heart attack or cancer, AF seldom kills immediately or over a short period. It has been likened to a slow poison in this regard.
Secondly, its very familiarity has bred contempt. Because AF is so common, physicians in the past may have been guilty of dismissing its importance. Some have held the view in the past that ‘AF is something you die with, rather than die of’.
Q. Well, are things improving now?
Yes, the true significance of AF has been recognised over the past 5 years. That is why the National Institute of Clinical Excellence (NICE) in the UK has published a separate guideline for AF in 2006 (here) and in 2007 the Department of Health linked payments to GP practices in England to their performance in managing AF.
Q. How does AF progress if left untreated?
In most patients, AF occurs initially in an intermittent fashion. In this stage of ‘paroxysmal AF’, patients get spells of AF for a few minutes to hours each time. Patients often experience palpitations during these spells, but as these spells are self-limiting, the condition is difficult to diagnose. The patient is in normal rhythm when seen by the physician, and his/ her symptoms are often dismissed as being due to anxiety or the like. Read this patient’s story for an example. As the disease progresses, AF episodes gradually become longer and more frequent. The second stage of ‘persistent AF’ is reached when the patient remains in AF all the time. Often this is the stage when the diagnosis is finally made and AF treated with external shock treatment and/or drugs. The third and final stage of ‘permanent AF’ is when the condition is so advanced that any attempts to restore normal rhythm prove futile. Although variable, it generally takes around 2-5 years for persistent AF to become permanent.
Q. How should AF be treated?
Every patient needs an individualised prescription, and so these are only broad generalisations.
-
1.Attempts should be made to decrease the risk of a blood clot forming (i.e., stroke) in all patients. This treatment may take the form of Warfarin, or one of a group of newer oral anticoagulants (NOACs, such as Dabigatran, Rivaroxaban or Apixaban) that do not require troublesome frequent blood tests for monitoring. Only those AF patients who are less than 65 years old AND who have no other medical condition other than AF are considered to be at low enough risk of stroke so as to not require treatment with blood-thinners.
-
2.Given the strong association between normal sinus rhythm and improved survival, consideration should be made to restoring normal rhythm in most patients. This strategy of ‘rhythm control’ may be applicable to the majority of patients with Paroxysmal AF and a large proportion of patients with persistent AF.
-
3.In patients with permanent AF and some patients with persistent AF, the alternative strategy of ‘rate control’ may be more appropriate. In this , the AF is allowed to continue but some of its harmful effects on heart function are reduced by slowing and regularising the heart rate. This may involve placement of a pacemaker.
-
Q.My doctor says that the ‘rhythm control’ strategy has not been proven to be better than the ‘rate control’ one?
This belief in some doctors is due to a few scientific studies which found these two treatment strategies to be equally effective. However, experts now believe that these studies had several severe limitations:
-
1.These studies were performed at the turn of the century when the rhythm control strategy involved only drugs and NOT catheter ablation. This is not reflective of current medical practice.
-
2.The drugs used to try and maintain normal rhythm proved ineffective in more than half the cases. This limited efficacy of drugs for treating AF severely jeopardised the rhythm control patients in comparative analysis.
-
3.The harmful side effects of these drugs caused an increased risk of death overall, which totally neutralised their beneficial effect in maintaining normal rhythm.
In fact, detailed analysis of these studies showed that presence of normal rhythm was strongly associated with a better survival rate. This stands to reason in terms of common sense as well and ties in with all large population based studies that have proven the strong association between AF and premature death.
As such, current scientific opinion is now agreeing on the fact that AF is a ‘bad’ condition to have, and that ‘rhythm control’ to normal sinus rhythm should be the ideal goal for all patients.
Q. What then are the treatment options for rhythm control?
Broadly, AF can be controlled with either drugs or catheter ablation. These two strategies are compared here
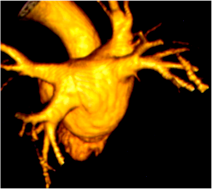




Left atrium
PV
PV
PV
PV
PV